ELISA Assay in COVID-19 Testing: Role and Reliability
Learn how this serological method aids in detecting antibodies and tracking immunity.

What is ELISA? Principles and Types
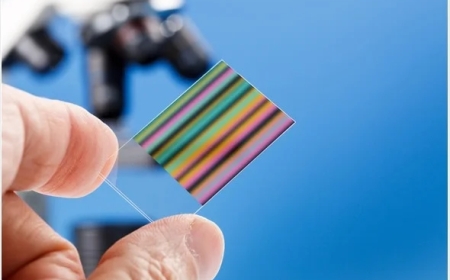
ELISA is a bioanalytical technique for the detection and quantification of biomolecules, such as proteins, hormones, and antibodies. The working principle of ELISA relies on highly specific antigen-antibody binding, followed by enzyme-based colorimetric detection.
Before we proceed to the application of ELISA in COVID-19 diagnosis, let us briefly look at the types of ELISA assays and the key advantages of ELISA analysis. ELISA immunoassay can be direct, indirect, sandwich, and competitive. The key steps in the ELISA lab assay involve antigen-antibody binding, followed by labeling an enzyme covalently to the antibody. Thereafter, the enzyme reacts with the substrate to produce a coloration, which is then quantified using a spectrophotometer.
Key advantages of the ELISA immunoassay include its high sensitivity, specificity, versatility, and capacity to perform qualitative and quantitative analysis. In addition, compared to singleplex immunoassays, multiplexed ELISA has several advantages, namely, high throughput, reduced sample requirement, improved efficiency in terms of time and cost, and enhanced reliability in detecting different protein molecules with a wide dynamic range. Thus, ELISA finds a wide range of applications, including diagnostic, research, and monitoring of diseases and therapeutic outcomes, such as quantifying antigens, antibodies, and Cytokine Analysis.
The ELISA assay is developed based on the application. The designed assay is optimized to achieve the desired sensitivity, accuracy, and specificity for detecting and quantifying the analysis. Thereafter, the assay undergoes validation by testing well-characterized reference samples, which serve as positive and negative controls. The ELISA validation is a crucial procedure that ensures the accuracy and reliability of the tool for its intended use.
Development of an ELISA Assay for COVID-19 Diagnosis
ELISA analysis is adapted to diagnose a wide range of viral diseases, e.g., HIV, Ebola, Hepatitis, and COVID-19, being the latest addition to the list. The SARS-CoV-2, causing COVID-19, has a genome of about 30 kilobases that encodes for multiple structural proteins: spike (S), envelope (E), membrane (M), nucleocapsid (N), along with other non-structural proteins. Among these proteins expressed, the S protein comprises two functional subunits, namely, S1 and S2, which help the virus attach to the host cell and fuse with the cell membrane. The S protein of the virus binds to the host cell through human angiotensin-converting enzyme 2 (ACE2). The N and S proteins, with their subunits, are most frequently targeted by diagnostic assays. ELISA, for example, targets the N-protein, S-protein, and S1 fragment of SARS-CoV-2, the causative agent of COVID-19, to detect the presence of antibodies produced in response to the infection.
Must Read: Future Trends and Challenges in the Field of Biochemical Assays
Developing an ELISA immunoassay for COVID-19 involves a few key steps. First, the viral antigens capable of eliciting an immune response within the host are determined. For SARS-CoV-2, researchers have identified S and N proteins as essential to the viral life cycle and have immunogenicity. These antigens are pipetted into the microtiter plates used for the ELISA lab. Recombinant proteins or peptide fragments from S and N proteins are added to coat the plates. The sample collected from the patient containing antibodies against SARS-CoV-2 is added to the plate and incubated. The immobilized viral antigens specifically bind to the antibodies. The plate is washed to remove any unbound material, and a secondary antibody linked to an enzyme is added to it. The secondary antibody complexes with the patients antibodies to form a complex, and the enzyme moiety catalyzes a reaction that is detected spectrophotometrically.
Most importantly, before developing the ELISA assay, the appropriate assay format needs to be chosen. The choice depends on the target antigen and antibody and the specificity and sensitivity of the assay required. Once developed, the assay needs to be optimized to maximize its performance as a diagnostic tool. Key factors to remember while optimizing the ELISA assay include viral antigen concentration, incubation time, blocking agents, and washing conditions.
Reliability of ELISA Assay as a COVID-19 Diagnostic Tool
Primarily, the ELISA assay serves as a reliable diagnostic tool to confirm the exposure of a person to SARS-CoV-2 by detecting the corresponding antibodies. ELISA-based COVID-19 diagnostic kits are commercially available with high sensitivity and specificity. Research indicates that ELISA assays outperform other methods, including lateral flow immunoassay, chemiluminescence enzyme immunoassay, and fluorescence enzyme-linked immunoassay in terms of diagnostic accuracy of SARS-CoV-2-linked IgG and IgM antibodies. When compared to highly sensitive techniques like PCR, studies suggest a high agreement between both for COVID-19 diagnosis.
However, the ELISA assay as a COVID-19 diagnostic tool is not without a few drawbacks. Despite being a reliable complementary test for COVID-19, it has limited capacity to predict the severity of infection and the clinical course of the disease. In addition, false positives are another concern in using the ELISA assay to diagnose COVID-19 infection. Thus, when using ELISA assay-based diagnostic kits, it is crucial to assess the onset of the symptoms and collect the samples appropriately. One should also analyze the results considering the potential limitations of the method and validate results with other methods, such as RT-PCR, if there are any discrepancies.